Medicine for attorneys: Spinal injuries
Understanding and presenting spinal/back And neck injuries at trial
Many personal-injury cases, especially those involving high-speed motor vehicle collisions, often deal with significant spinal injuries. However, even a lower-velocity impact can result in spinal conditions which negatively affect the quality of a person’s life and will need to be explored in trial. Imaging such as MRIs are an extremely helpful tool to identify spinal injuries, but are not the only consideration. Physical exams, patient complaints and diagnostic treatments are also needed to fully grasp the nature and extent of spinal injuries.
There are various types of spinal injuries, for which diagnosis can generally be made with the use of X-rays, MRIs and CT scans. However, many spinal injuries originally go undiagnosed by emergency medical treaters, and plaintiffs are commonly sent home after a crash to rest and use ice/heat. Further, the full scope of spinal injuries cannot be solely identified with imaging alone. Therefore, imaging should not be singularly relied on; rather, plaintiff’s subjective complaints, physical exams and treatment results should all be considered.
This article shall serve as a helpful primer for what to analyze when a client comes in with certain complaints and how to appropriately guide them to proper medical treatment so their condition and case can be fully understood. Further, presenting these issues at trial commonly requires a strong grasp of medicine, likely treatment modalities, future outlook and use of demonstrative evidence.
Types of common spinal injuries from impact events
Many motor vehicle crashes will result in some muscle strain, commonly referred to as “whiplash,” which may resolve with conservative care. However, based on a person’s pre-existing condition of their spine and severity of the forces imparted, more serious and permanent conditions frequently occur.
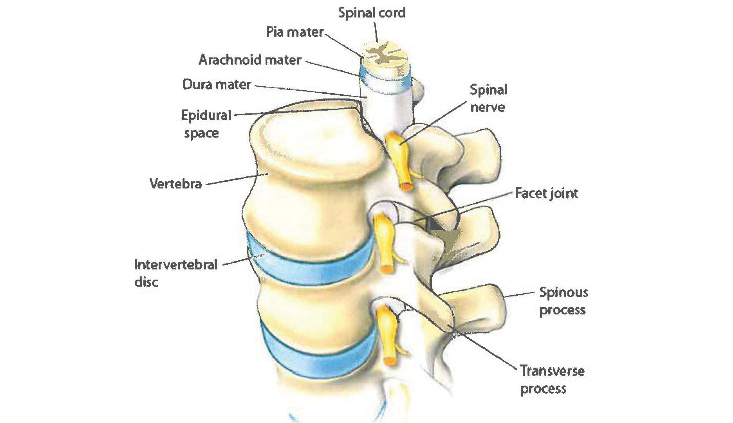
The spine is made up of 24 individual vertebrae which are stacked on each other, forming the spinal column. The spine is divided into three regions, cervical, thoracic and lumbar. Cervical contains the upper vertebrae, C1-C7, thoracic contains the mid vertebrae, T1-12, and the lumbar contains the lowest vertebrae, L1-L5.
These vertebrae each have a circular hole center which contains and protects the spinal cord. The other side of the vertebrae have multiple bony processes that jut out from the rear and to the sides, the spinous process and the transverse process. The facet joints branch off from each vertebra and connect together, holding the vertebrae stable and forming a joint to allow for extension and flexion movements. Ligaments, tendons and surrounding muscle also provide additional stability and movement for the spine column.
Also running through the vertebrae are nerve roots that act to carry messages from the brain to the rest of the body through 31 pairs of nerve roots. The nerve roots travel through a small opening between vertebrae, called foramina, to connect to specific parts of the body. Depending on the location of the nerve in the region of the spine, the nerve can relay messages to specific areas of the body, including the upper extremities, trunk and lower extremities. Jelly-like pillows that sit between the vertebrae, called discs, provide insulation and absorb pressure for the vertebrae. When a physically traumatic event occurs, each of these components can become injured and cause pain and limitations. Below is a summary of the most common spinal injuries we frequently deal with in a personal injury matter.
Fractured vertebrae
A strong force applied to the spine can cause the vertebrae to break, in one or many places depending on the force applied. Often, surgical intervention for fractured vertebrae is not medically advised and many of these fractures can heal without invasive intervention. However, if the vertebrae are pushed out of place due to the break such that it is considered “unstable” and may affect the spinal cord, there is a much more increased likelihood that surgery will be required. Depending on the location of the break, other areas of the vertebrae may be affected, causing a myriad of symptoms, including pain, limited motion and radiculopathy down the limbs if the nerves are impacted. X-ray imaging is frequently adequate to identify this type of condition, however an MRI and/or a CT scan may be required to give treaters greater insight into the other areas around the fracture.
With regard to car crashes, a person wearing a seatbelt during a motor vehicle collision may experience fractured vertebrae if the top of their body jerks forward while their low body is restrained back. Interestingly, women are more predisposed to experience spinal fractures than men, as are adults over 50 years of age. Osteoporosis in particular may make this more likely to occur. If a plaintiff is an older adult, especially one with osteoporosis, this type of injury can occur even with low delta-v forces, and can be easily missed by emergency medical providers that may assume a muscle strain is the only injury present. Further, if not diagnosed in time, the fracture can fuse improperly, rendering proper correction impossible.
Annular fissures
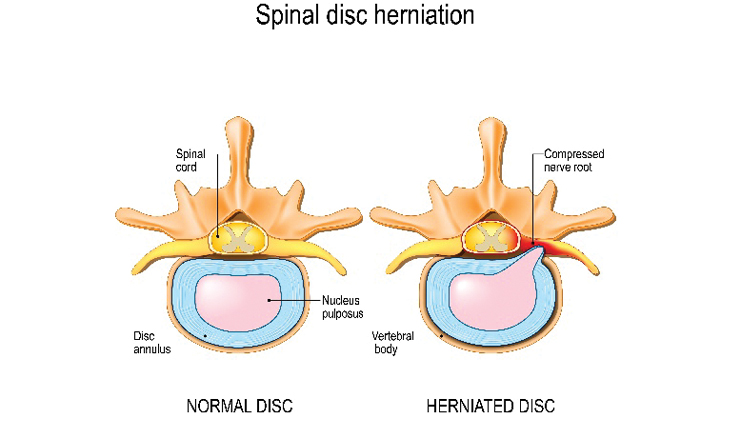
Discs, the jelly-like substance providing a cushion between the vertebrae, are composed of two parts: the soft center, the nucleus pulposus, and an outer ring, the annulus. The annulus is made out of tough connective tissue that serves to encircle and protect the fluid- filled inner nucleus. The annulus provides a framework for the disc, maintaining its shape and integrity, while the nucleus provides shock absorption.
A plaintiff may experience tears or fissures to the annulus due to degenerative changes or trauma. Sometimes, annular tears will not be painful but could evolve into becoming painful if the tear grows. If an annular fissure is located near a nerve root, the nerve root can become irritated, resulting in pain and radiating symptomology. If severe enough, the annular tear can allow the fluid in the nucleus to leak, causing a disc herniation or bulge. Therefore, as they can often be progressive, these conditions need to be monitored with repeat imaging until stabilized.
Both MRI imaging and CT scans can be used to diagnose and assess annular fissures. An MRI is often the best tool as an annular fissure will appear brighter compared to the surrounding annular fibrosus due to an increase in water content at the tear. Although a CT scan provides less detail than an MRI in this regard, a CT scan can still identify compression to the nerve root or spinal cord, suggesting an annular fissure.
Disc herniations and bulges
When a disc herniates, a tear in the annulus allows the nucleus to leak out. This fluid then extrudes beyond the disc area, resulting in a herniation. The increased fluid can interfere with other processes in the spinal canal, including the nerve root or spinal cord. Herniated discs can occur at any region of the spine, and the location of the herniation generally results in both pain in that area and numbness, tingling or weakness down the related extremities.
Disc herniations can be caused by disc degeneration or traumatic events. As a person ages, the discs become more dehydrated, resulting in greater propensity to tear and herniate. Thus, although annular fissures may be present prior to an impact, an older plaintiff is more likely to experience a disc herniation due to the weakened state of their discs.
Conversely, with a disc bulge, the annulus protrudes outward beyond the natural margins of the disc but does not tear to the nucleus. Although nucleus fluid is not leaking externally into the spinal canal, the bulge can still compress an adjacent nerve root, causing pain.
Frequently, the signs of a disc herniation or bulge may not be present immediately after a motor vehicle collision or other injury event. Plaintiffs often experience a progressive worsening of their pain following a collision as the disc continues to tear and leak, which can occur over a period of hours to weeks. An MRI is generally used to identify the presence of a disc herniation or bulge.
Facet injuries
As described above, the vertebrae are joined together with facet joints that connect, providing stability and flexibility to the spinal column. These facet joints are small sliding joints that contain cartilage to lubricate the motion. Often, these delicate facet joints can become injured when a plaintiff is subjected to forces as their spine is twisted or extended, like when looking in a side mirror. Due to the nature of facet joints, facet injuries can occur even at low delta-v forces, a fact that the defense regularly overlooks.
Trauma, including a motor vehicle collision, can cause the facet joints to develop arthritic changes and inflammation, reducing the lubricating cartilage, and causing osteophytes as well as joint inflammation. All these conditions can result in irritation to the joint itself as well as the adjacent nerves.
Frequently, facet injuries can mimic many of the signs present in a disc herniation or bulge. Other times, facet pain does not follow a nerve root pattern and can be difficult to pinpoint. Plaintiffs can often feel localized pain in the area, radiating pain, stiffness, and pain that increases with bending, twisting or stretching. However, unlike a disc bulge or herniation, facet injuries can be difficult to diagnose with imaging, particularly in the cervical spine. Therefore, frequently a facet joint injection can be a treatment modality as well as a diagnostic tool – if the patient experiences significant pain relief, it confirms the existence of the facet injury.
Additionally, it is not uncommon for a person who has injured discs to also experience facet arthropathy. When a disc experiences loss of disc height, the vertebrae compress onto each other, putting additional pressure on the facet joints. This increased pressure can cause significant wear and tear to the joints over time, increasing the injury to the spine and providing another likely source of future pain. Should this occur, a plaintiff who was successful with treatment modalities geared to initial injury may later experience an evolution in their complaints of pain and require divergent treatment to other areas as their condition continues to deteriorate.
Radiculopathy
When an injury to the disc results in compression to the surrounding nerve roots, a plaintiff will likely experience radiating symptoms into the related extremity. The type and area experiencing radiculopathy is dictated by the affected nerve root. Cervical radiculopathy commonly presents with pain, weakness, numbness and tingling beginning at the neck and out to the arms. Thoracic radiculopathy may create pain around the chest. Lumbar radiculopathy can result in these symptoms traveling from the low back and into the lower extremities. Radiculopathy can often be confirmed on MRI imaging, to assess the conditions of the discs around the nerve root(s) at issue and an Electromyography (EMG), which measures the electrical impulses to determine how a nerve is functioning.
Treatment modalities
Each condition requires a specific and individualized care plan based on the plaintiff’s personal history and symptoms. With that said, treatment following a traumatic event, barring injuries requiring hospitalization, often follow similar trajectories.
Initially following a collision, people presenting for emergency evaluation are physically examined and sent for an X-ray. Usually, they are diagnosed with muscle strain, prescribed muscle relaxers and/or over the counter anti-inflammatories and sent home to rest. Should their pain continue, people frequently proceed with either chiropractic treatment or physical therapy. If this conservative treatment is unsuccessful at permanently reducing the pain, the injured plaintiff is then frequently sent for an MRI of the affected area. Should the MRI demonstrate spinal injuries, the plaintiff is referred to specialist care, frequently an orthopedic specialist, pain management specialist and/or neurosurgeon. Based on the review of the findings of the MRI and the plaintiff’s needs, conservative care may be further explored or they may proceed with more invasive options.
Many times, in litigating a personal- injury case, the defense will assert that spinal injuries are pre-existing and/or due to degenerative changes rather than the event at issue. For instance, many defense experts assert that low delta-v impact collisions cannot result in spinal injuries. However, this fails to take into account the nuance of the circumstances of each collision. Although some may not incur chronic spinal conditions in low-speed impacts, depending on the individual plaintiff, the pre-existing conditions of their spine and their positioning during the crash, it is possible for these injuries to occur. (Michael D. Freeman PhD, MPH, DC, Christopher J. Centeno, MD, Sean S. Kohles, PhD, A Systematic Approach to Clinical Determinations of Causation in Symptomatic Spinal Disk Injury Following Motor Vehicle Crash Trauma, American Academy of Physical Med. & Rehab., Vol. 1, 951 (October 2009).)
Additionally, a plaintiff’s complaints of neck or back pain prior to the collision are frequently held up as an example of a pre-existing injury. However, a prior complaint of pain does not defeat causation. If a plaintiff has a prior MRI from before the event, comparing the prior images with imaging taken post-crash is the gold standard for demonstrating a new or worsened condition.
For a plaintiff who has had past lower-back pain, drawing a distinction between the absence of radiculopathy prior and following the collision can be helpful to show worsening of the condition. For instance, a plaintiff may have a prior history of cervical pain, however they never complained to their treaters of numbness, tingling or weakness before. Following the impact, they then experienced radiculopathy down their bilateral arms, indicating an evolution of their pre-existing condition. The closer the temporal relation between the event in question and the new symptoms or complaints, the stronger the assertion that the collision is the causal factor. (Freeman, supra, at 952-953.) This relationship can demonstrate that while the plaintiff had some prior conditions that caused pain, the crash in question worsened the injury and caused irritation to the nerve root, suggesting an increased disc bulge or herniation.
Many people do not experience significant neck or back pain until a trauma event, and then are sent to receive their first imaging of the affected spinal region. Frequently, when an MRI is performed, the imaging can show some amount of disc degeneration. A significant portion of the public has disc degeneration, especially most people over the age of 50, however this condition is often asymptomatic unless triggered by a later event. Studies have shown that following a motor vehicle collision, people with mild to moderate low-back pain are much more likely to experience incidence of recurrent pain in the future. (Paul S. Nolet, Vicki L. Kristman, Pierre Cote, Linda J. Carroll, J. David Cassidy, The association between a lifetime history of low-back injury in a motor vehicle collision and future low-back pain: a population-based cohort study, Eur Spine J (2018) 27:136-144, 140.) Therefore, an understanding of both the current condition of a plaintiff and their likely future outcomes is necessary to adequately predict future damages and medical needs.
Epidural steroid injection
Frequently, the first procedure provided to a plaintiff with intractable pain and positive imaging results will be an epidural steroid injection into the affected area. These injections act to deliver strong anti-inflammatory medicine to the space surrounding the nerve roots. This injection both numbs the area and reduces inflammation, resulting in decreased irritation to the nerve root. A plaintiff can sometimes achieve permanent pain relief with a singular epidural, particularly if the decreased inflammation allows them to proceed with a strengthening regimen to develop supportive muscles and posture changes to accommodate the spinal region at issue. However, more commonly, the epidural will need to be repeated approximately every 6 to 18 months, as the efficacy wears off.
When presenting at trial, an explanation of what an epidural injection did for the plaintiff’s condition as well as the need to repeat the procedure regularly needs to be included in any discussion of future care. A plaintiff’s seemingly “pain-free” demeanor while at trial may also be explained to the jury by a recent epidural injection. This should include discussion by plaintiff’s treaters and plaintiff themself regarding the positive results of the injections and the pain that would be present if the injections were not performed – highlighting their need for repeated procedures.
Facet joint injections/medial branch blocks
Unlike epidural steroid injections to the vertebral epidural space, facet joint injections target the facet joints if the joints are the likely source of the pain. Similarly, a medial branch block injects steroids into the medial branch nerve that transmits pain impulses from the facet joints.
As stated above, facet joint injuries can be difficult to diagnose on imaging and even if seen, injuries to the facet joints may or may not be the actual source of pain. Therefore, a facet joint injection and a medial branch block is both treatment and diagnostic tool. When this injection is performed, if a plaintiff does not feel substantial relief in the subsequent few days, the injected facet joints are not the likely source of pain.
Further, facet joint injections and branch blocks generally have very temporary benefit, commonly fading after a few weeks. Therefore, these injections need to be frequently repeated to provide relief.
Radiofrequency ablation
Should the strength of the facet injections fail to control plaintiff’s facet pain sufficiently, the plaintiff may be considered a good candidate for radiofrequency ablation, which can provide longer-lasting relief. Radiofrequency ablation targets the medial branch nerve but uses energy to “burn” the nerves so that they cannot transmit pain signals. Although this procedure intentionally damages the nerves, for many people their nerves will regrow, requiring repeat procedures every year or so.
It is important to note that many people find this procedure relatively painful in comparison to injections. In trial, exploring the methodology of radiofrequency ablation and the discomfort the procedure causes are often necessary to highlight the continued suffering of the plaintiff.
Spinal surgery
Should a spinal injury, like a disc herniation, be severe enough, surgery may be required. A discectomy removes the damaged portion of a herniated disc surgically, whereas a laminectomy surgically addresses issues with vertebrae. Often, these procedures are performed concurrently, as a discectomy may result in movement of the affected disc that can irritate adjacent nerves and part of the vertebra may need to be removed to accommodate the nerve root following this shift.
If a disc is too damaged, the disc at issue can be fully removed and replaced with an artificial disc. Generally, an artificial disc replacement procedure is a viable option if a patient has pain that does not adequately respond to less invasive options due to two vertebrae compressing upon each other due to a damaged disc, rather than multiple discs at issue. Should there be significant fractures and/or vertebral arthritis, particularly to the facet joints, spinal fusion may be the only option. A spinal fusion surgically stops the motion between vertebrae by installing implants or other devices to fuse the components together. This can result in a reduction of pain, but also results in limited mobility of the area where the procedure occurred and there are some risks of complications.
Spinal surgery is always a last resort, particularly for a young patient, and reflects a severe spinal injury. Recovery outcomes are generally good, however, there are more risks including spinal weakness and increased risk of future herniation.
Presenting at trial
Spinal injuries can be complex to present at trial and confusing for juries. Most lay people are unfamiliar with the anatomy of the spine and associated nerves. Unfamiliar vernacular and a lack of black and white rules can result in overwhelmed jurors that are unsure of which side to believe. Therefore, when presenting these issues at trial, a well-prepared plaintiff’s attorney can both educate the jury and earn their trust by simplifying the issues presented.
First, counsel presenting a case at trial often engage in a “battle of the experts,” where each side’s experts vehemently argue and disagree. Jurors are often savvier than many attorneys realize and are skeptical of these “hired gun” experts. As counsel representing the plaintiff, you have the added benefit of speaking with, and preparing and eliciting testimony of, the plaintiff’s treaters for deposition and trial.
A treater who has overseen and directed the plaintiff’s care, who can speak to their condition, treatment and future outlook presents much more legitimately to the jury. If multiple treaters all provide supportive testimony regarding their care and opinions, this is difficult for the defense to defeat with their paid-for experts.
Particularly with spinal injuries, demonstrative evidence is very helpful to explain to the jury important aspects of the plaintiff ’s case. Some people are visual rather than auditory learners, and, although we attorneys may find trial exciting, it is frequently boring for others. Therefore, visual representations of the injuries can hold the attention of jurors and allow them to better understand the medicine at issue.
These visual representations can cover a myriad of topics in the case, including bio-mechanical re-creations showing forces imparted on the spine, imaging of the injury and/or explanations of treatment modalities. In particular, with impacts involving lower delta-v forces and/or facet joint injuries, a re-creation showing the exact twisted position and movement of the plaintiff’s body at the point of impact can illuminate how even a low-speed impact caused such damage.
Stills from MRIs and CT scans are also difficult to understand unless viewing with a trained eye. Due to this, the imaging can be enhanced to highlight the area at issue and show the jury convincing proof of injury they can see for themselves. Further, demonstrative re-creations of the treatment modalities, for instance an epidural injection, ablation procedure, or spinal surgery, can also hammer home what the plaintiff must now endure to treat their spinal injury.
It is important to note that demonstrative evidence can easily be excluded at trial if the proper foundation is not adequately laid. A treating doctor can be provided demonstrative evidence at deposition and can be asked to confirm that certain records accurately depict the injury or treatment. It is particularly effective if the treater is asked to use the demonstrative evidence to explain a certain issue, and then add their own notations. Highlighted aspects of medical imaging, including X-rays, MRIs and CT scans, can be admitted when accompanied by foundational authentication for its admissibility. (Sinz v. Owens (1949) 33 Cal.2d 749, 759.) Once a foundation is appropriately laid, these substantiated records and additional drawings can then be utilized by an expert witness for their own opinion without running afoul of the ruling in People v. Sanchez (2016) 63 Cal.4th 665.
Conclusion
Spinal injuries are regularly encountered in personal injury cases and a plaintiff’s attorney needs to be well versed in recognizing the injuries, suggest proper care, assess damages and explain these injuries at trial. Simplyfying the complexities through demonstrative presentation, including anatomy drawings, imaging, crash re-creations and treatments, can help the jury make sense of the issues. Treating doctors can be a valuable resource both to present the cause and extent of these injuries and lay a proper foundation for this demonstrative evidence.
Olivia K. Leary

Olivia K. Leary is a member of the Rains Lucia Stern St. Phalle & Silver, PC Personal Injury Group. She represents people who have suffered serious injury as a result of automobile accidents, defective products, dangerous premises, negligence, and intentional torts.
Eustace de Saint Phalle

Eustace de Saint Phalle is a partner with Rains Lucia Stern St. Phalle & Silver, PC in San Francisco. He manages the personal injury practice for the firm statewide. The firm’s personal injury practice focuses on civil litigation in a variety of areas, including industrial accidents, product liability, exceptions to workers’ compensation, premises liability, professional malpractice, auto accidents, maritime accidents and construction defect accidents.
Copyright ©
2025
by the author.
For reprint permission, contact the publisher: Advocate Magazine